My Deep Dive into Figuring Out This Excipient Lung Thing
Honestly, this whole “excipient lung disease” term just popped up for me last month. Saw it mentioned somewhere vague about folks having breathing troubles potentially linked to stuff added to pills or vaccines. Figured I’d dig in since it sounded weird and kinda scary. Barely knew squat when I started.
First thing I did was hit up my usual medical sources online. Big mistake. Wall of text, complicated doctor talk, felt like banging my head against a wall. I needed something real, something step-by-step. So I shifted gears and started hunting down stories. Real people. Who actually got diagnosed? How did it happen?
Turns out, it’s messy. Like, way more messy than I expected. Seems like a huge puzzle piece is the patient’s story – what medicines they took, what vaccines they got, especially weird new ones. Docs really need to ask about every single little pill or shot, which sounds simple but probably gets missed a lot.
Okay, so they suspect it. Now what? Apparently, they gotta rule out tons of other junk that looks just like it. This is where I got lost at first. What tests? Found out:
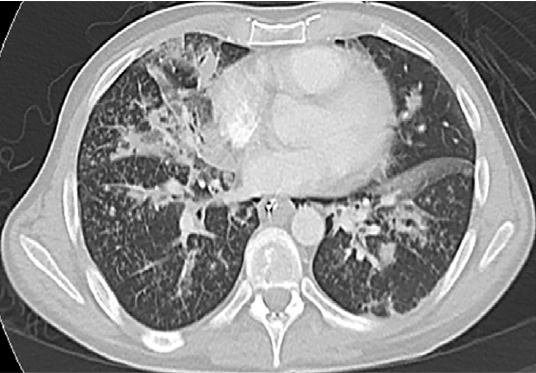
- Chest pictures are key. Like CT scans. They look for these strange patterns deep in the lungs that aren’t just your regular pneumonia.
- Slicing tiny bits of the lung?! Yeah, biopsies. Seems drastic, but sometimes it’s the only way to see those specific weird cell reactions doctors associate with the filler ingredients causing trouble.
- Scoping the lungs. Bronchoscopy. They sneak a camera down there to peek around and sometimes suck out fluid to test. Sounds awful.
Putting this all together felt like trying to assemble IKEA furniture without the instructions. Why? Because often, the doctors won’t find the actual excipient culprit just floating around in the test samples. It’s mostly gone! They’re looking at the mess it left behind and matching that mess to the patient’s history of swallowing or injecting pills/shots.
Total headache trying to grasp the diagnostic chain. It wasn’t a neat “Step A leads to Step B” thing. More like:
- Person gets seriously weird breathing problems.
- Doc hears “Hey, I started this new med/vaccine around when this started…”
- Doc freaks out internally cause it might be this rare excipient thing.
- Then starts the frantic scramble:
- Look at chest scans hard.
- Maybe try not to give the suspect med anymore to see if things improve.
- Shove a camera down the throat (yikes!).
- Maybe carve off a tiny lung piece (double yikes!).
- Stare endlessly at tissue samples.
- Rule out infections and every other lung disease under the sun.
- Finally, if the lung damage pattern fits AND the exposure history fits AND nothing else does… maybe then they call it excipient lung disease.
What did I really learn? It’s detective work. Hard detective work. Docs need a sharp eye, patience, and a willingness to ask very specific questions about every little thing a person put in their body. It’s easier just to call it regular pneumonia or asthma and call it a day. Figuring out this specific thing feels like finding a needle in a haystack made of other needles. Felt like an idiot half the time wading through it, but hey, now I kinda get the basics. If nothing else, it sure makes me read the “inactive ingredients” list more carefully now!